
The first and only dedicated Neuroradiology Department developed as Integral part of Neurosurgery at Lahore General Hospital in 1970. Neuro-endovascular treatment for CCF, carotid stenting, aneurysm (coiling) AVM & Dural AVF (embolization) was started in 2003 which has saved more than 9800 lives since then. For the first time in Pakistan Aneurysms are being coiled within 48 hours of rupture preventing re-bleeding and dreadful complications which has drastically decreased morbidily and mortality due to subarachnoid haemorrhage.
A brain aneurysm, also called a cerebral or intracranial aneurysm, is a weakened area of an artery in the brain which causes a bulging or ballooning of part of the vessel wall. Aneurysms form silently due to wear and tear process of arteries, and sometimes can form from injury, infection, or inherited tendency. Aneurysms occur in all age groups, but the incidence increases steadily in individuals of 25 and older, are most prevalent in ages 50 to 60.
Unruptured Brain aneurysms are often asymptomatic, particularly when they are small. Large unruptured aneurysms may cause symptoms based on the pressure they put on surrounding structures, including brain tissue or nerves. Unruptured aneurysms are not less frightening or life threatening than ruptured aneurysm, and may require treatment depending upon size, risk of haemorrhage and other factors.
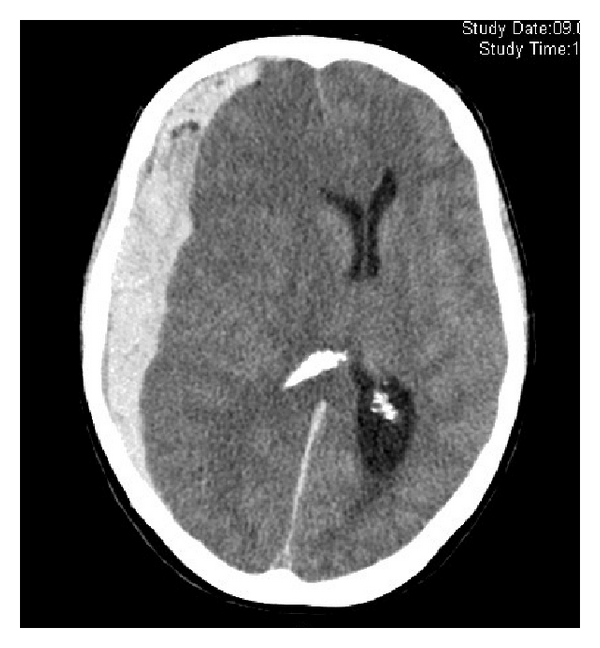
When cerebral aneurysms rupture, they usually cause bleeding into the brain or the space closely surrounding the brain known as the “subarachnoid space”. Blood can irritate, damage, or destroy nearby brain cells. Each year approximately 2% to 3% of people with a brain aneurysm suffer from bleeding. Ruptured brain aneurysms are fatal in about 50% of cases.
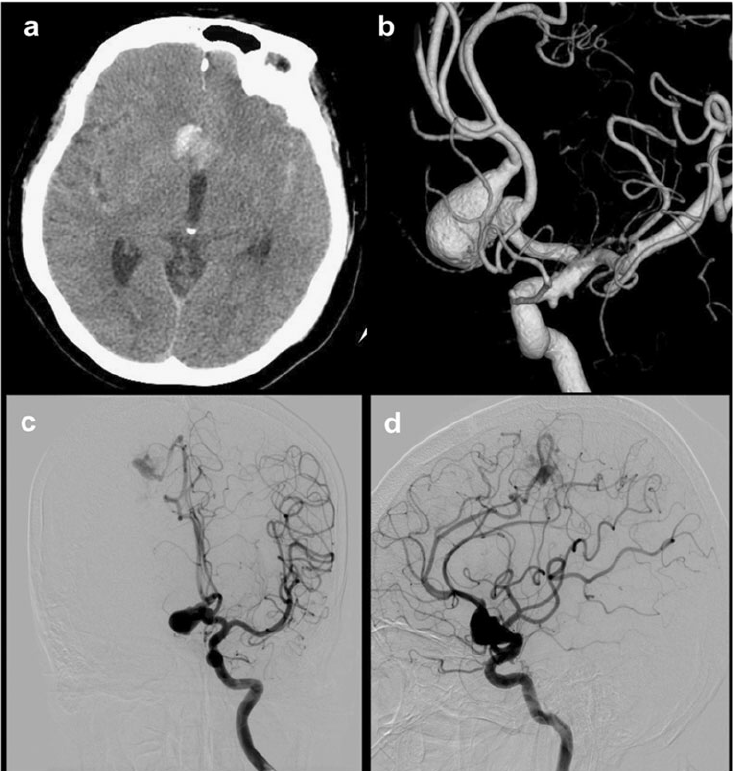
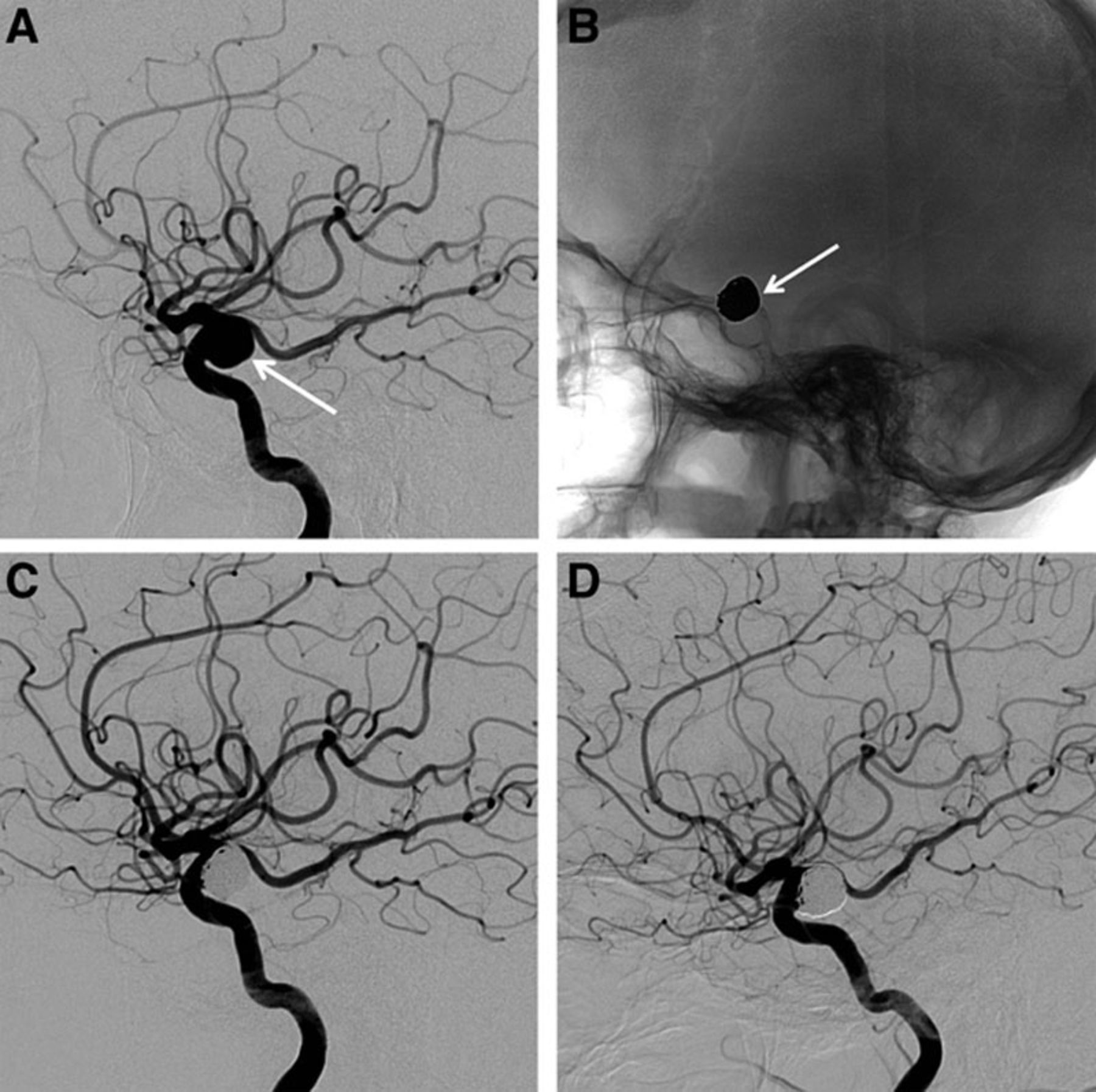
Aneurysms can be diagnosed in several different ways. Diagnosis of a ruptured cerebral aneurysm is typically made by finding signs of subarachnoid hemorrhage on CT Scan followed by CTA or MRA or DSA. To determine the exact location, size and shape of an aneurysm, a neurointerventionalist will perform a test called a cerebral angiogram (DSA).
Today there are two treatment options for people who have been diagnosed with a brain aneurysms. ‘ Surgical Therapy (craniotomy) known as aneurysm clipping * Endovascular Therapy known as aneurysm coiling It is important to note, however, that not all aneurysms are treated at the time of diagnosis or are amenable to both forms of treatment. Patients need to consult a neurovascular specialist to determine if they are candidates for either treatment.
In 1937, Walter Dandy, MD, introduced the method of “clipping” an aneurysm by applying a small, V-shaped silver clip to the neck of an aneurysm. An operation to “clip” the aneurysm is performed by doing a craniotomy (opening the skull surgically), and isolating the aneurysm from the bloodstream and placing one or more clips across the neck of the aneurysm.
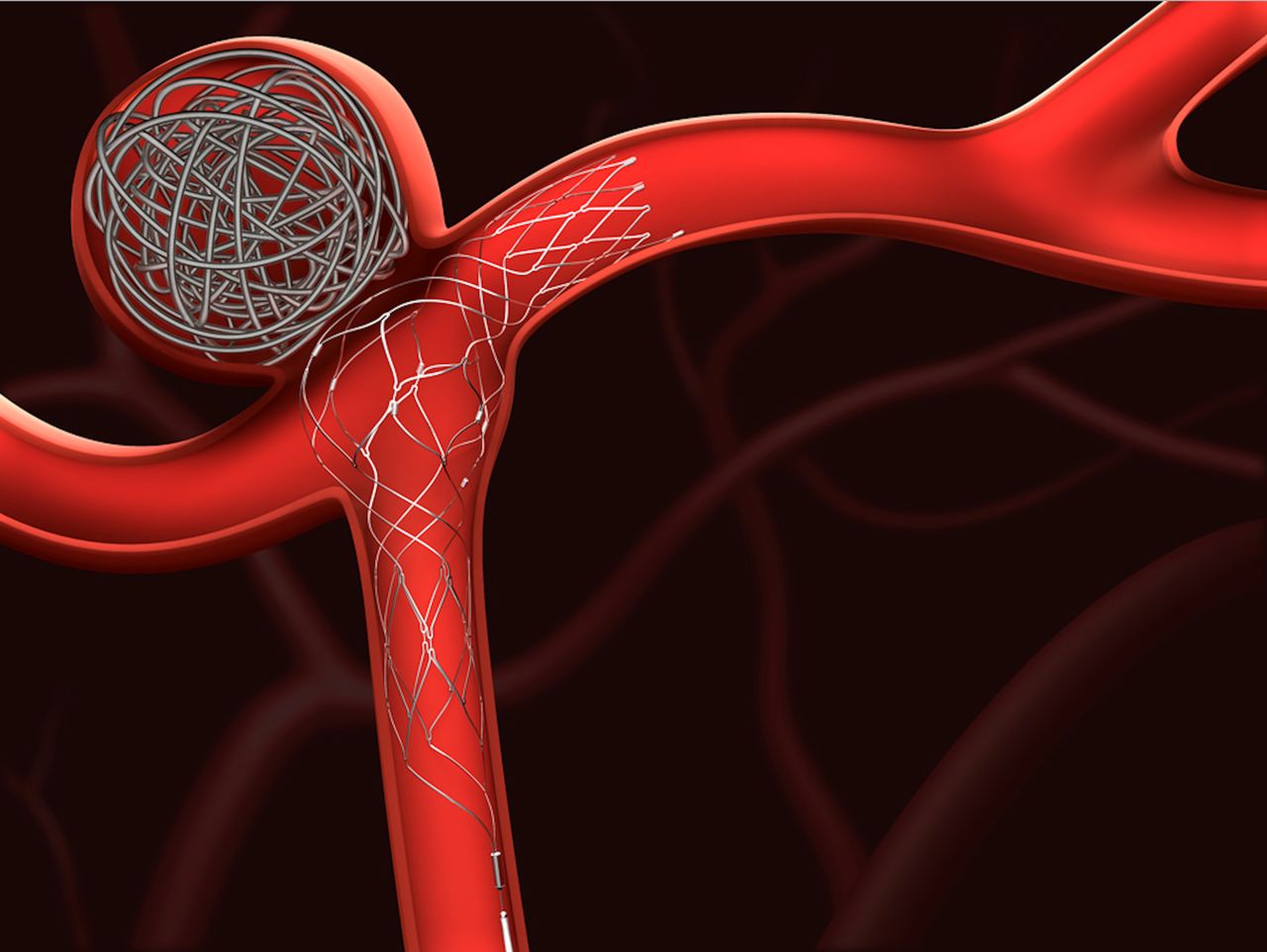
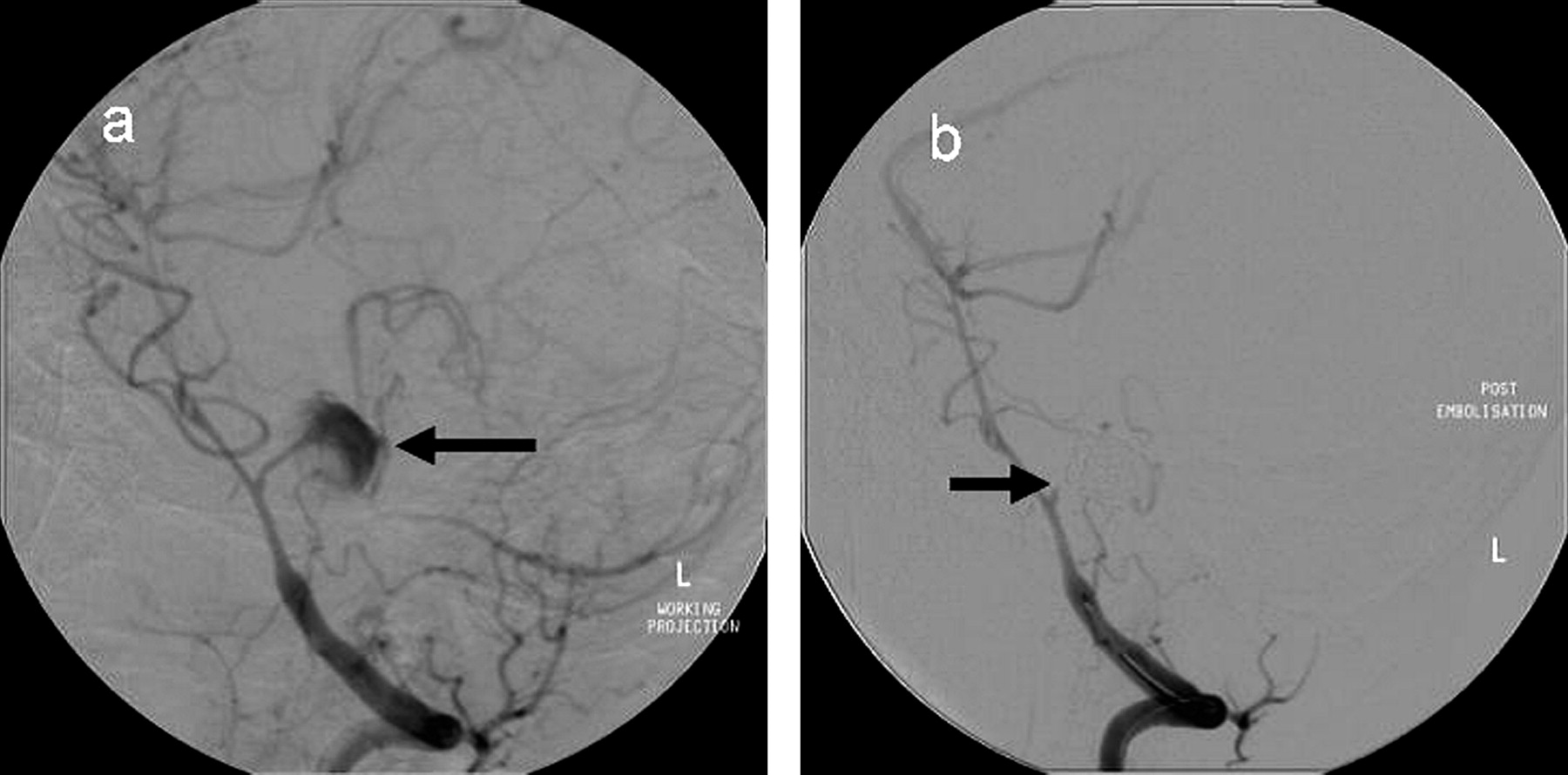
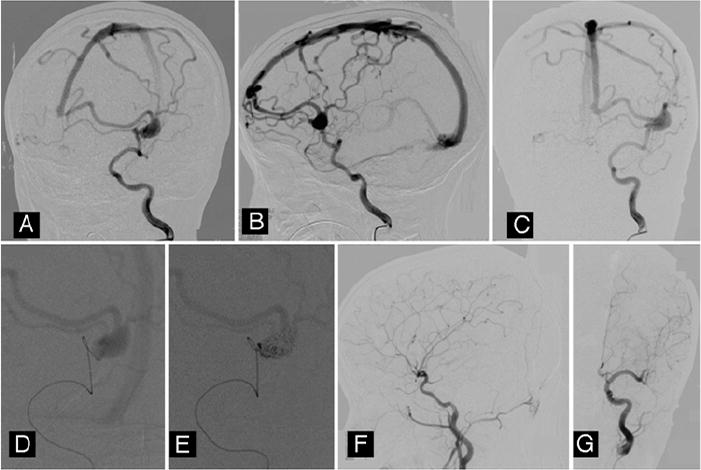
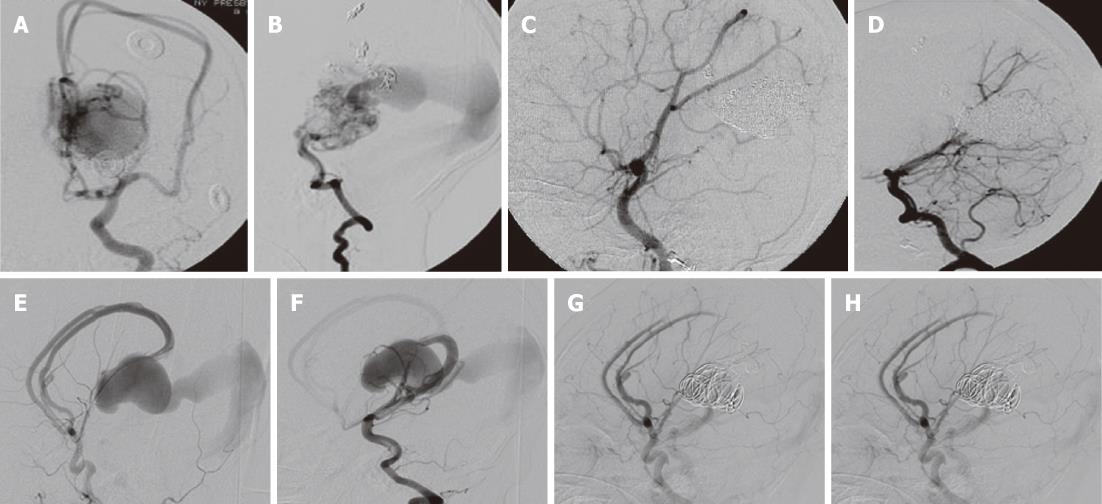
A less invasive technique called endovascular coiling, which does not require a craniotomy, uses microcatheters to deliver small coils into the aneurysm in order to occlude (fill) the aneurysm from inside the blood vessel.
Endovascular coiling dates back to the development of the Guglielmi Detachable Coil System (GDC) which was approved by the FDA in 1995.
The GDC Detachable Coil revolutionized endovascular treatment of aneurysms. Coils are deposited into the aneurysm via a microcatheter which is typically inserted into a groin artery and navigated through the neurovascular system to the location of the aneurysm.
Once the coils are released into the aneurysm, the blood flow pattern within the aneurysm is altered. The stagnation of this blood flow usually leads to thrombosis (clotting) of the aneurysm.
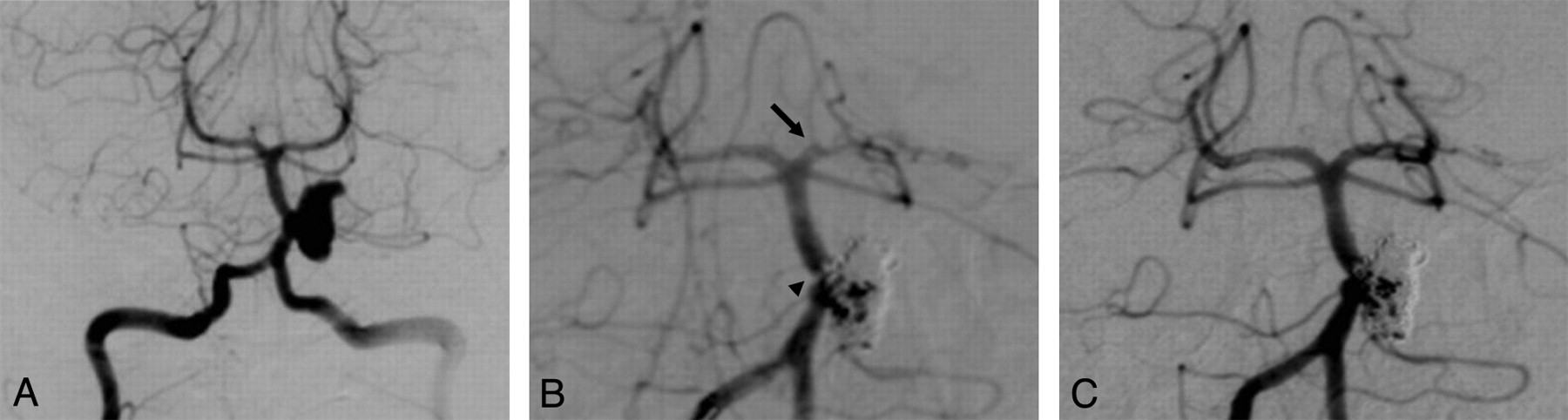
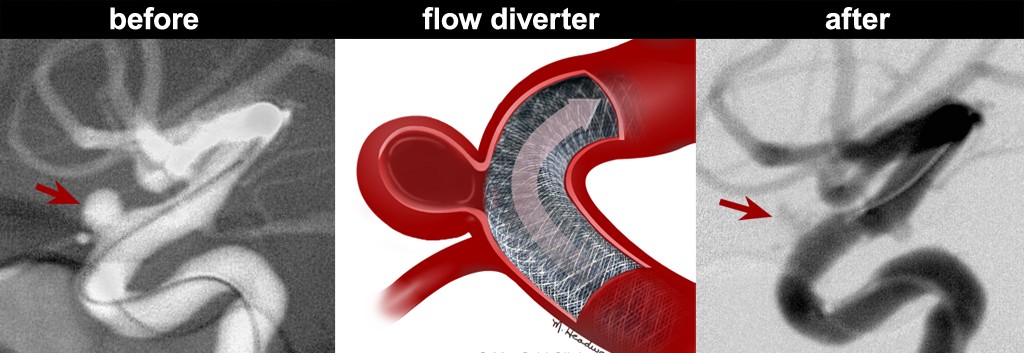
Endovascular coiling sometimes requires the use of an additional devices such as balloon assisted, stent assisted or only flow divertor(FD).
This device enables treatment of a broader neck of aneurysm that may be difficult to treat with coils alone. Stenting with coiling utilizes a small flexible cylindrical mesh tube that provides a scaffold for the coiling.
The Anu after endovascular coiling Angiogram of an aneurysm before treatment. It has been filled with treatment. The aneurysm is the dark coils preventing further blood flow bulge on the vessel. into the aneurysm.
End0vascular coiling is performed by a trained neuro-interventionalist. A neurointerventionalist has specialized training not less than 5 years in nuroscience, neuroimaging, endovascular techniques for the brain and spine.
While the best method of securing the aneurysm should be determined on individual basis, in general, patients with a ruptured cerebral aneurysm should be treated as soon as possible. Surgical risks and outcomes depend on whether or not the aneurysm has ruptured, the size and location of the aneurysm, and the patient’s age and overall health.
Although the frequency of certain complications may vary, both clipping and coiling have risks. Aneurysm rupture is the most serious complication in both treatments. Rupture can cause intracerebral haemorrhage (bleeding into the brain), subsequent coma or death. Ischemic stroke, which is a stroke caused by small emboli in the bloodstream, is also a potential risk of either treatment.
Results from the International subarachnoid Aneurysm Trial (ISAT), a randomized clinical trial which compared surgical clipping to endovascular coiling in the treatment of ruptured aneurysms. were published in the Lancet in 2002. The study found that in patients equally evocable for both treatment options, endovascular coil treatment is showed better patient outcome than surgery in terms of survival free of disability at one year. The relative risks of death or significant disability at 1 year for patients treated with coils was 23.5% lower than in surgical-treated patients. The study results were so compelling that the trial was halted early because the trial steering committee determined it was no longer ethical to randomized patients to clipping. Long-term follow-up from the ISAT trial was published in 2009. The risk of death at five years was significantly lower in the coiled group than in the clipped group. Long-term follow-up from the ISAT trial was published in 2009. The risk of death at five years was significantly lower in the coiled group than in the clipped group.
Although no multi-center randomized clinical trial comparing endovascular coiling and surgical treatment of unruptured aneurysms has yet been conducted, retrospective analysis found that endovascular coiling is associated with less risk of negative outcomes, shorter hospital stays and shorter recovery times compared with surgery.
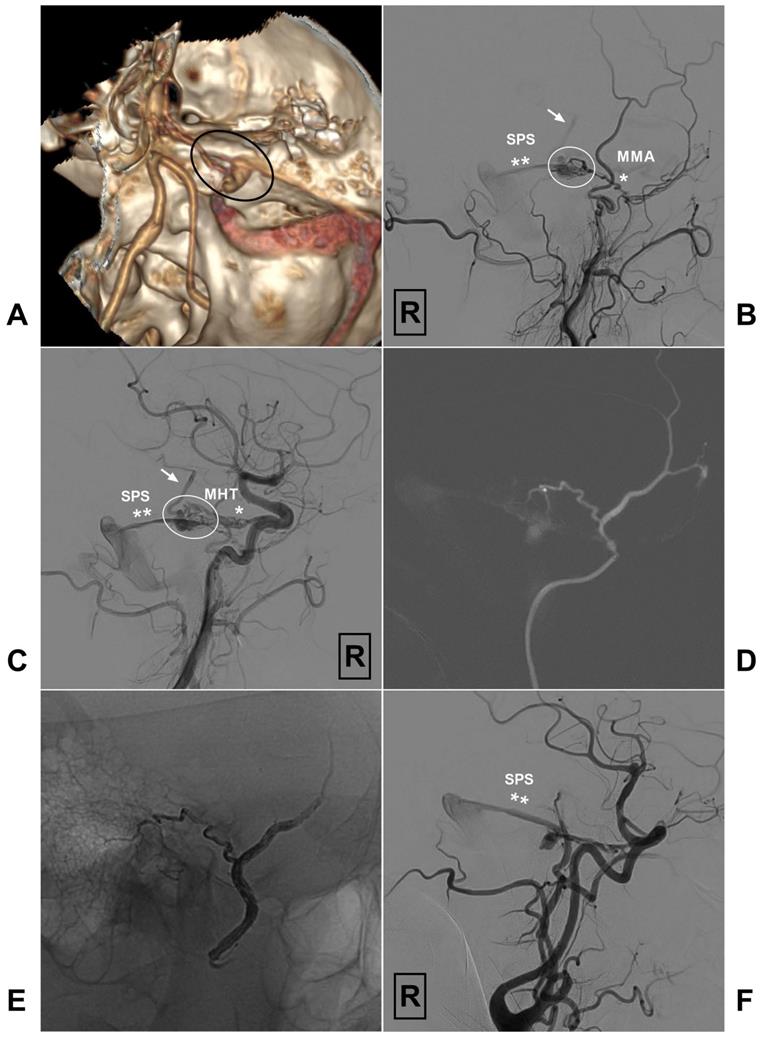
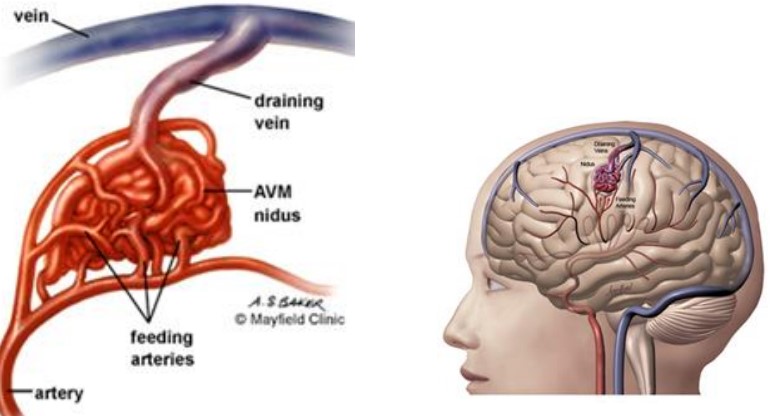
PAVF are rare vascular malformations that usually consist of a single dilated pial artery connecting directly to an enlarged cortical draining vein
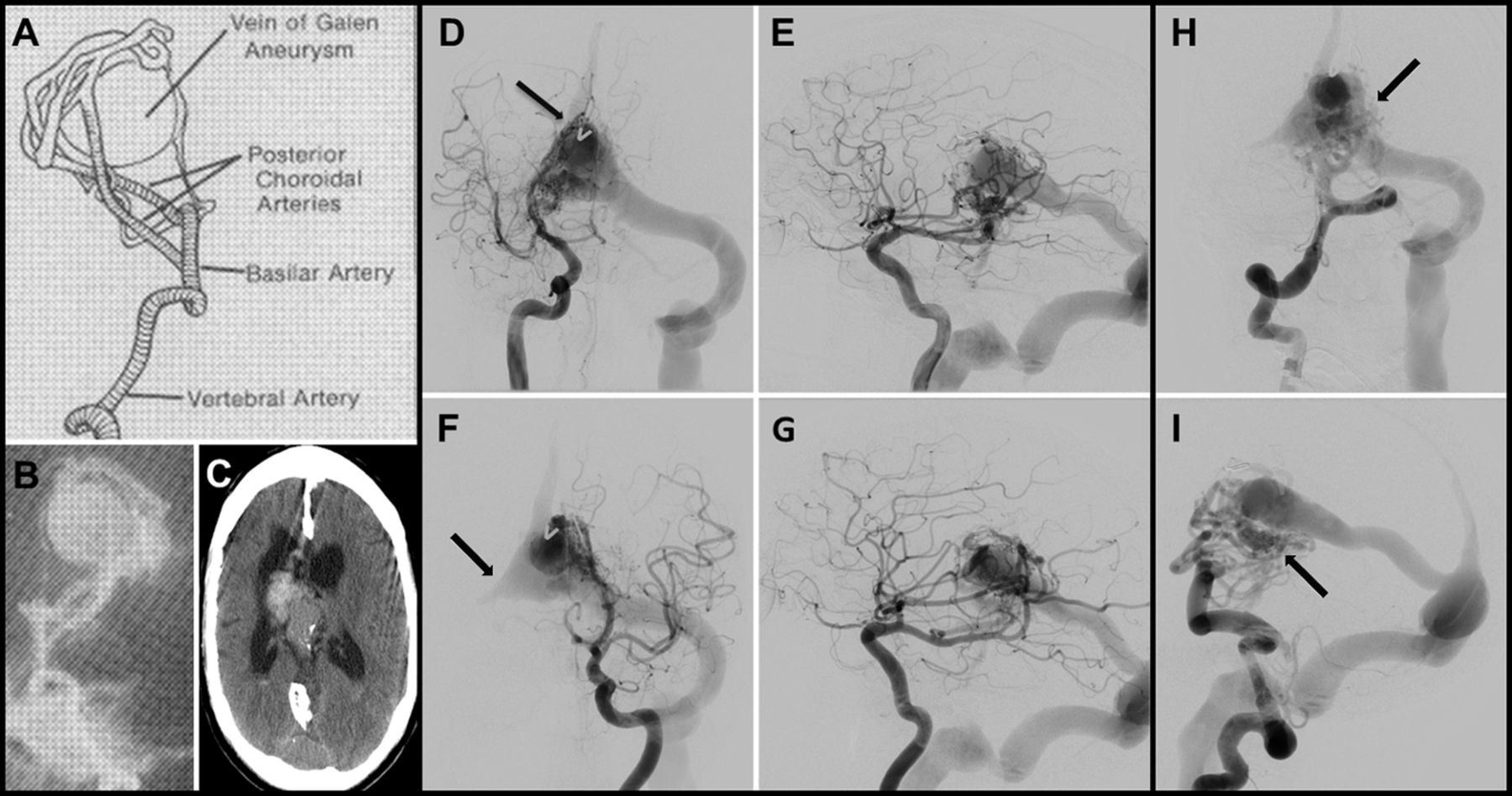
| Differential Characteristics | Choroidal VGAM | Mural VGAM |
|---|---|---|
| Vein of Galen Afferents | No | No |
| Dorsal Vein of the prosencephalon | Yes | Yes |
| Falcine Sinus | Frequent | Possible |
| Communication with Cerebral Veins | No | No |
| Most Frequent age of consent | Newborn | Infant |
| Cardiac Manifestations | Almost Constant | Frequent |
| CSF Disorders | Frequent | Frequent |
| Failure to Thrive | Yes | Possible |
| Expected rate of cure per type with E | High | Very High |
| Natural History | Unknown | Unknown |
| Risk of Future hemorrhage | If distal dural sinus thrombosis | If distal dural sinus thrombosis |
| Risk of Future Focal Neurological Symptoms | If Ventricular shunting or calcification | If Ventricular shunting or calcification |
Error: Contact form not found.
In case of Emergency Call +92 300 4270130
Lahore General Hospital Lahore Pakistan
+92-301-4857-543
info@ntarcp.com
